Vitamin D deficiency: what you need to know


Vitamin D deficiency: what you need to know
To help you understand Vitamin D deficiency, we've put together this guide.
What is vitamin D?
Vitamin D is essential for building strong bones and optimising calcium absorption from the gut (1). It also has roles in maintaining a healthy immune system, skin and muscle strength (1). Despite its importance, approximately 31% of Australians are deficient (2).

Where do you find Vitamin D?
Vitamin D occurs in two forms. Vitamin D3 or Cholecalciferol is produced by the action of sunlight on the skin (1). Vitamin D2 or Ergocalciferol is found in some foods (1). However, there are limited food sources with significant amounts of this important nutrient. As a result, it is almost impossible to obtain sufficient from diet alone (1).
In Australia, margarine and some milk are fortified with vitamin D. Other sources include eggs and fatty fish such as salmon, herring and mackerel (1). Some studies suggest that mushrooms, when exposed to ultraviolet (UV radiation) can also generate vitamin D (3).
Vitamin D from the sun
The main source of this vitamin is sunlight. The body is designed to synthesise vitamin D when bare skin is exposed to sunlight. The key component of the sun’s rays that is important for this process is ultraviolet B (UVB) (4). This happens in 15 minutes for a fair-skinned person or a couple of hours for a dark-skinned person (4).
There are several factors that affect how much vitamin D is synthesised (4):
- The time of day: The skin can synthesise greater amounts when exposed during the middle of the day.
- Location: The distance away from the equator affects exposure. People living closest to the equator can produce the highest amounts of vitamin D.
- Skin colour: Pale skin tones synthesise faster than darker skin.
- Amount of exposed skin: Exposing a large surface area of the skin increases the production capacity.
Due to the high prevalence of cancer in Australia, the Cancer Council recommends covering up with clothing and going into the shade for optimal sun protection (5).

How much Vitamin D do you need each day?
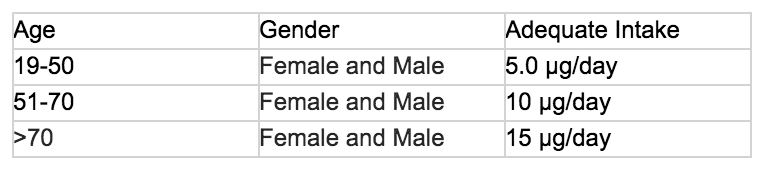
The amount of vitamin D required each day increases with age. One study assessed the synthesis rate in older women with fair skin. It found that exposure to sunlight on the face, hand and forearm for 15-30 minutes, 2-3 times per week provides the equivalent of 15 μg per day (6).
Signs of Vitamin D deficiency
In deficiency, the body is unable to build and mineralise bones. When this occurs in young children, it can lead to a condition known as rickets (1). This causes bowed legs and knocked knees (1).
In adults, deficiency can lead to osteoporosis, a condition where bones become porous and brittle (7). Deficiency has also been linked to other conditions such as osteomalacia, secondary hyperparathyroidism and an increased risk of fractures (1).
Emerging research suggests that this vitamin may also play a role in the prevention and treatment of many conditions. These include cancer, heart disease, diabetes and neurodegenerative diseases (8,9,10).
Who is at risk of Vitamin D deficiency?
Those with risk factors for deficiency include (1,2,4,7):
- Young children at rapid periods of growth with low calcium intake.
- People who wear overprotective clothing.
- Office workers or those with limited exposure to the sun.
- People who have undergone weight loss surgery such as gastric sleeve or bypass.
- People who live in countries with limited sunlight.
- People with darker skin. This is due to the melanin pigment in dark skin, not absorbing as much UV radiation as fair skin.
- Older adults and disabled people in low-level and high-level residential care.
- People with medical conditions or medication that affects vitamin D metabolism. This includes liver and kidney disease, cystic fibrosis, coeliac disease and inflammatory bowel disease.
- People with diets very low in fat.
- Babies or infants of vitamin D deficient mothers. This is particularly at risk if the babies are partially or exclusively breastfed.

How do you test vitamin D deficiency?
If you are concerned about your levels, it is important to seek advice through your GP. The main method of testing levels is through a blood test. This will test the main form circulating in the body, known as 25-hydroxyvitamin D (7). To optimise bone health, the recommended levels in the blood should be greater than 50 nmol/L (7).
How do you treat vitamin D deficiency?
For people with vitamin D deficiency, it is essential to improve blood levels through a vitamin D supplement (7). The supplement should be titrated based on the level of deficiency. A high dose is required with severe deficiency. It can take between three to five months from commencing supplementation before the full increase in blood levels are seen (7). Blood levels should also be assessed three months after commencing treatment to assess and maintain adequate vitamin D levels (7).
Should I take a vitamin D supplement?
If you do not get adequate full-body exposure to sunlight or are in a high-risk category, it may be important to consider a supplement. Vitable’s Vitamin D and Calcium Plus supplements provide a source of vitamin D to support bone and immune health. Take the quiz here today.

Find out more about other areas that the above supplements can help you with:
*Always read the label. Follow the directions for use. If symptoms persist, talk to your health professional. Vitamin and/or mineral supplements should not replace a balanced diet.
References
- Nrv.gov.au. (2019). Vitamin D | Nutrient Reference Values. Published on: https://www.nrv.gov.au/nutrients/vitamin-d
- Daly, R., Gagnon, C., Lu, Z., Magliano, D., Dunstan, D., Sikaris, K., Zimmet, P., Ebeling, P. and Shaw, J. (2012). Prevalence of vitamin D deficiency and its determinants in Australian adults aged 25 years and older: a national, population-based study. Clinical Endocrinology, 77(1), pp.26-35.
- Cardwell, G., Bornman, J., James, A. and Black, L. (2018). A Review of Mushrooms as a Potential Source of Dietary Vitamin D. Nutrients, 10(10), p.1498.
- Vitamin D Council. (2019). How do I get the vitamin D my body needs?. [online] Available at: https://www.vitamindcouncil.org/about-vitamin-d/how-do-i-get-the-vitamin-d-my-body-needs/#.XSOhM5MzagQ [Accessed 8 Jul. 2019].
- Cancer Council Australia. (2019). Pubslished on: https://www.cancer.org.au/
- Kimlin, M., Downs, N. and Parisi, A. (2003). Comparison of human facial UV exposure at high and low latitudes and the potential impact on dermal vitamin D production. Photochemical & Photobiological Sciences, 2(4), p.370.
- Osteoporosis.org.au. (2019). Published on: https://www.osteoporosis.org.au/sites/default/files/files/Vit%20D%20Position%20Statement%2010%202013%20V2(1).pdf
- Ford, J., MacLennan, G., Avenell, A., Bolland, M., Grey, A. and Witham, M. (2014). Cardiovascular disease and vitamin D supplementation: trial analysis, systematic review, and meta-analysis. The American Journal of Clinical Nutrition, 100(3), pp.746-755.
- Gaksch, M., Jorde, R., Grimnes, G., Joakimsen, R., Schirmer, H., Wilsgaard, T., Mathiesen, E., Njølstad, I., Løchen, M., März, W., Kleber, M., Tomaschitz, A., Grübler, M., Eiriksdottir, G., Gudmundsson, E., Harris, T., Cotch, M., Aspelund, T., Gudnason, V., Rutters, F., Beulens, J., van ‘t Riet, E., Nijpels, G., Dekker, J., Grove-Laugesen, D., Rejnmark, L., Busch, M., Mensink, G., Scheidt-Nave, C., Thamm, M., Swart, K., Brouwer, I., Lips, P., van Schoor, N., Sempos, C., Durazo-Arvizu, R., Škrabáková, Z., Dowling, K., Cashman, K., Kiely, M. and Pilz, S. (2017). Vitamin D and mortality: Individual participant data meta-analysis of standardized 25-hydroxyvitamin D in 26916 individuals from a European consortium. PLOS ONE, 12(2), p.e0170791.
- Koduah, P., Paul, F. and Dörr, J. (2017). Vitamin D in the prevention, prediction and treatment of neurodegenerative and neuroinflammatory diseases. EPMA Journal, 8(4), pp.313-325.
